CMS’ Patient-Driven Payment Model (PDPM) will take effect October 1, 2019, replacing Resource Utilization Groups (RUGs) for Medicare Part A fee for service payment to skilled nursing centers. Payment is based upon an array of patient characteristics, primarily medical information, associated with newly designed direct care components. Administrators, reimbursement, clinical and coding staff all need an understanding of the PDPM, as it represents a fundamental shift in how care is delivered and centers are reimbursed.
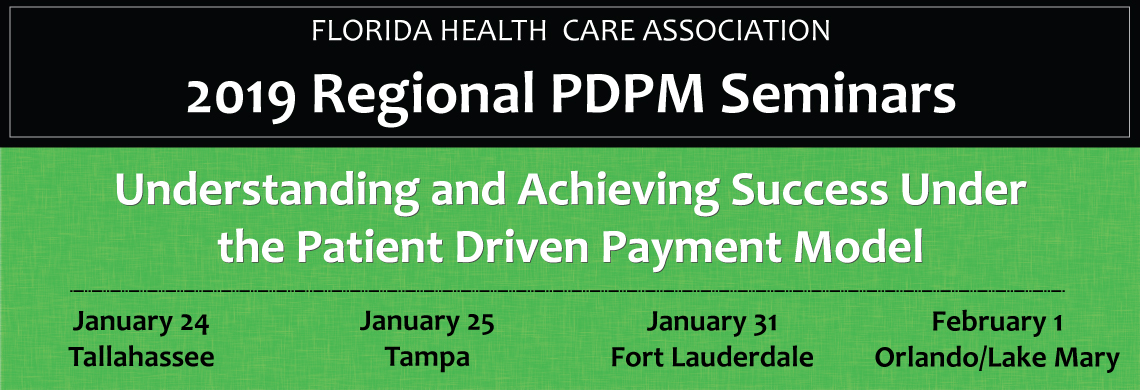
FHCA’s Regional PDPM Seminars will help providers understand the PDPM and learn how to achieve success under the new payment system, including how to lower costs, optimize your reimbursement and improve patient outcomes. A bonus session on reducing hospital readmissions will cover steps that providers can take to improve their readmission score and maximize their Medicare revenue.
Attendee Information
Nursing home administrators, nurse leaders, social workers, therapists, consultants, medical directors, financial and reimbursement specialist, MDS, Coders, admission directors and business office managers will benefit from these seminars.
- Download the Attendee Brochure
- Download Presenter Handouts (password protected for registered attendees only)
- Click here to complete a brief, online evaluation by March 1 to be entered into a drawing for a chance to win a $100 VISA gift card.
Continuing Education
An official online continuing education report of your contact hours will be available by February 15, 2019, on the MTS Tracking website. To ensure accurate reporting, please review the online continuing education report to verify your contact hours and license number before February 20, 2019.
FHCA will submit contact hours (based on scan records) to CE Broker by February 22, 2019, for transmission to the Florida Department of Health.
Approved for Six (6) hours of continuing education – Provider Number 50-720: Florida Board of Nursing Home Administrators, Florida Board of Nursing, Florida Board of Clinical Social Work and the Florida Board of Occupational Therapy. Contact FHCA at (850) 224-3907 or info@fhca.org with any questions.
Learner Objectives
- Gain a broad understanding of the new Medicare PDPM and how it is different than the current RUGs model.
- Learn how the correct MDS and ICD-10 coding is imperative to being adequately reimbursed.
- Understand how to operationalize new reimbursement changes at the provider level to be successful.
- Review the importance of contracting and implementing agreements with therapy companies.
- Cover strategies on how to reduce re-hospitalizations in order to maximize Medicare revenue under value-based purchasing.
Sponsors
Thank you to all our sponsors who helped make this event possible. Click here for a complete list of sponsors per training location.
Sponsorships are sold out for these seminars. Contact Jenny Early at jearly@fhca.org to learn more about future sponsorship opportunities.